Tuberculosis affects millions of Filipinos, yet remains misunderstood.
Key Takeaways
- Majority of Filipinos know that coughing is a symptom of TB, and that coughing for several weeks is a more specific indicator for possible TB.
- Only one-fifth of Filipinos know that TB is caused by bacteria, but majority know that smoking is a key risk factor.
- Only 8% know that TB is exclusively airborne, and not spread through saliva.
- Almost all know that TB can be cured.
- There is much to do in improving awareness and perceptions about TB.
The Philippines is one of the countries contributing the most to the global burden of tuberculosis (TB), and it is very far from achieving the Sustainable Development Goal (SDG) on TB. National prevalence surveys on TB are conducted regularly, and the latest one was completed in 2016. There is also a law (RA 10767 passed in 2015), focusing on TB elimination, together with a clear strategy document called the Philippine Strategic TB Elimination Plan (PhilSTEP, Phase 1 is being implemented from 2017 to 2022), and a manual of operations (MOP) instructing health care providers on TB case management.
Given all of this, little is known what Filipinos actually understand about TB, particularly its signs and symptoms, causes, and method of transmission. The 2013 and 2017 DHS has multiple questions regarding basic facts on TB, which are summarized as follows.
Awareness of TB signs and symptoms
Persistent coughing, specifically coughing for at least two weeks, is one of the symptoms used for screening of presumptive, or possible, TB. The World Health Organization (WHO) rates the specificity of this symptom in screening TB as high, meaning that the presence of persistent cough is a good sign that one needs to seek a doctor for possible TB. In fact, one recent Department of Health (DOH) and United States Agency for International Development (USAID) ad campaign focused on this.
In both 2013 and 2017, 9 out of 10 Filipinos mentioned that coughing is a symptom of presumptive TB. What is interesting between the two years is that more respondents specifically mentioned that the coughing needs to occur over several weeks (34% in 2013, 56% in 2017). The question on signs and symptoms of TB is unprompted, so it is interesting to see that a lot of Filipinos are more aware that the cough needs to be persistent for it to raise suspicion of TB.
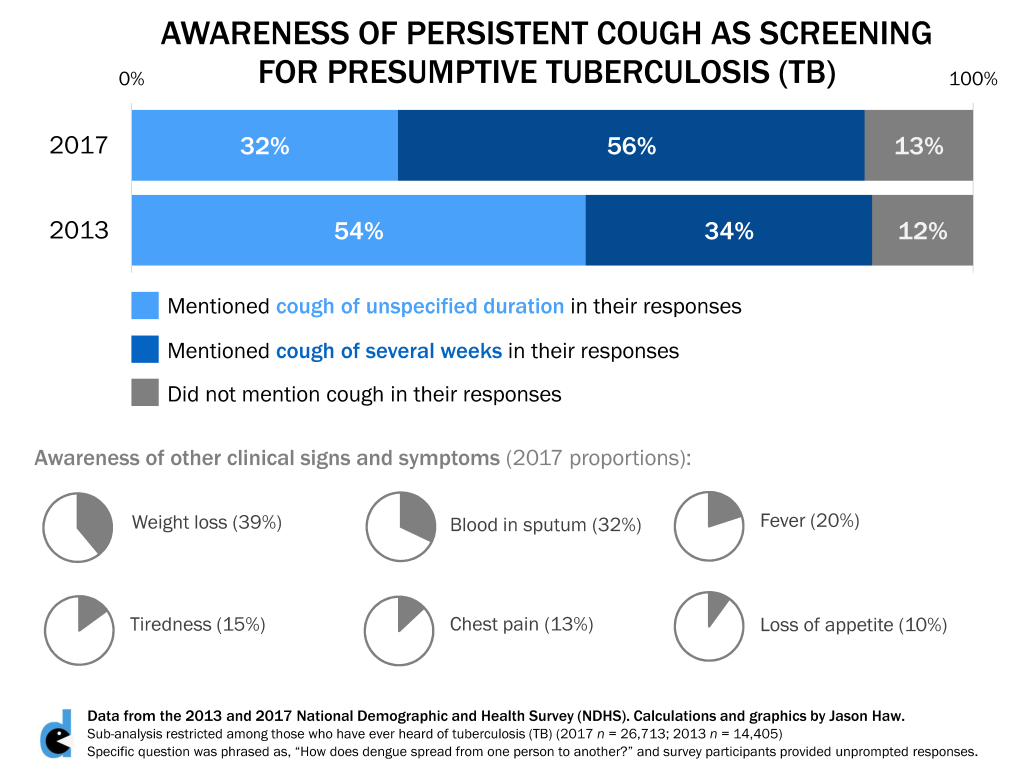
Other symptoms were not as familiar – weight loss was mentioned by 4 out of 10, presence of blood in sputum was mentioned by 3 out of 10, and other symptoms were much less mentioned.
Knowledge on TB causes and risk factors
Respondents were asked to provide top-of-mind answers of what they thought were the causes of TB. The categories in the survey were a bit vague, and the concept of causation in public health is not black and white. One may think that a certain biological agent is the primary cause of any infectious disease, but other social determinants may play a role in causing the disease as well, whether directly and indirectly.
With this, the results are presented as follows:
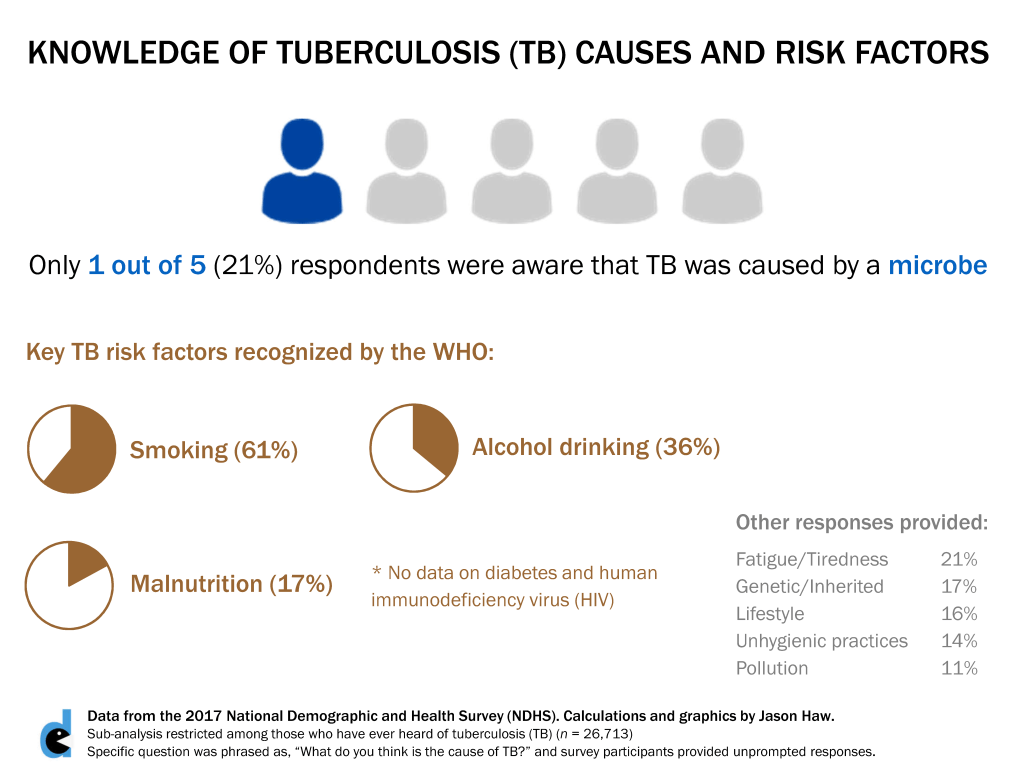
Only 1 out of 5 respondents in both 2013 and 2017 mentioned microbe as a cause. The specific microbe was not recorded anymore in the survey but for everyone’s information, it is Mycobacterium tuberculosis.
The WHO lists five key risk factors (one can interpret this as plausible causes) of TB: smoking, harmful alcohol drinking, malnutrition, diabetes, and being human immunodeficiency virus (HIV)-positive. There were no data available on the last two, as a result of no respondent reporting unprompted responses of these, probably. For the rest, smoking was mentioned by about two-thirds, alcohol drinking by about one-third, and malnutrition by around one-sixth of respondents.
Misconceptions on TB Transmission
When respondents were asked about how TB was spread, only 8% were correct in saying that it was airborne. Specifically, it is prolonged exposure to cough droplets by a TB-infected person. It is not spread through saliva (e.g. sharing utensils and food, or even kissing), as answered by an overwhelming 88% of respondents.
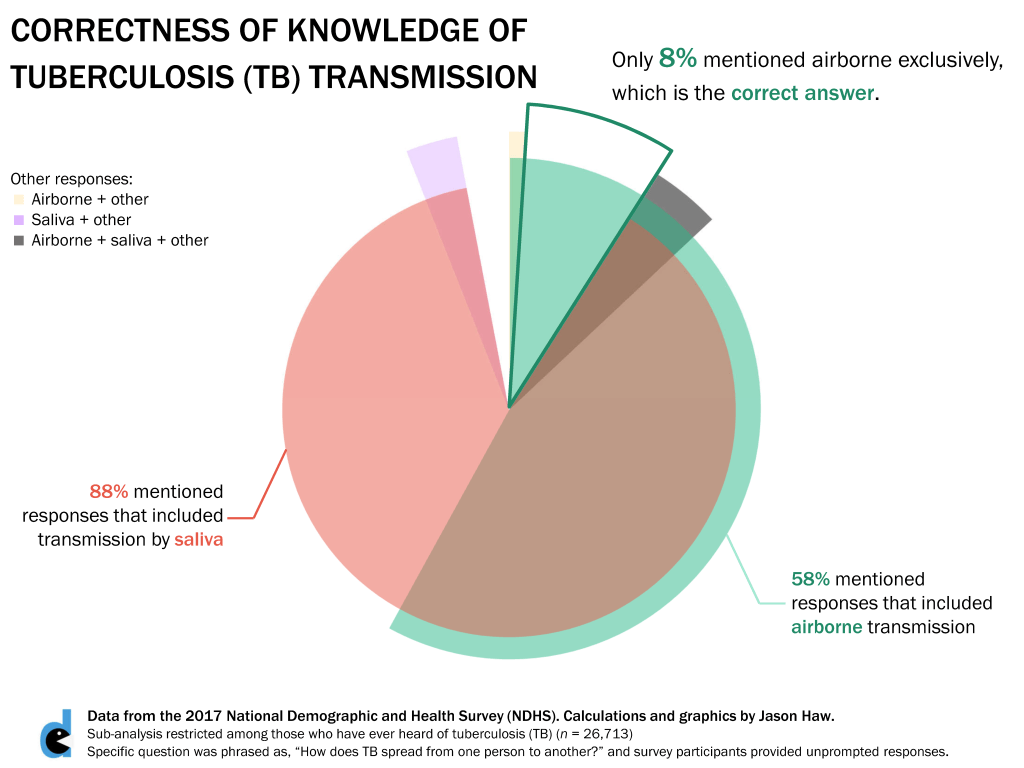
The results are worrying. This means that most Filipinos do not understand how TB is spread, and it may affect how they deal with someone with TB and the precautions they need to take. While more than half of the respondents did mention airborne transmission, majority also thought that transmission by saliva was also possible.
Perceptions on TB
Finally, three questions about TB perceptions were asked as a Yes/No question. Almost everyone thought that TB can be cured, with the proportions being the same between 2013 and 2017.
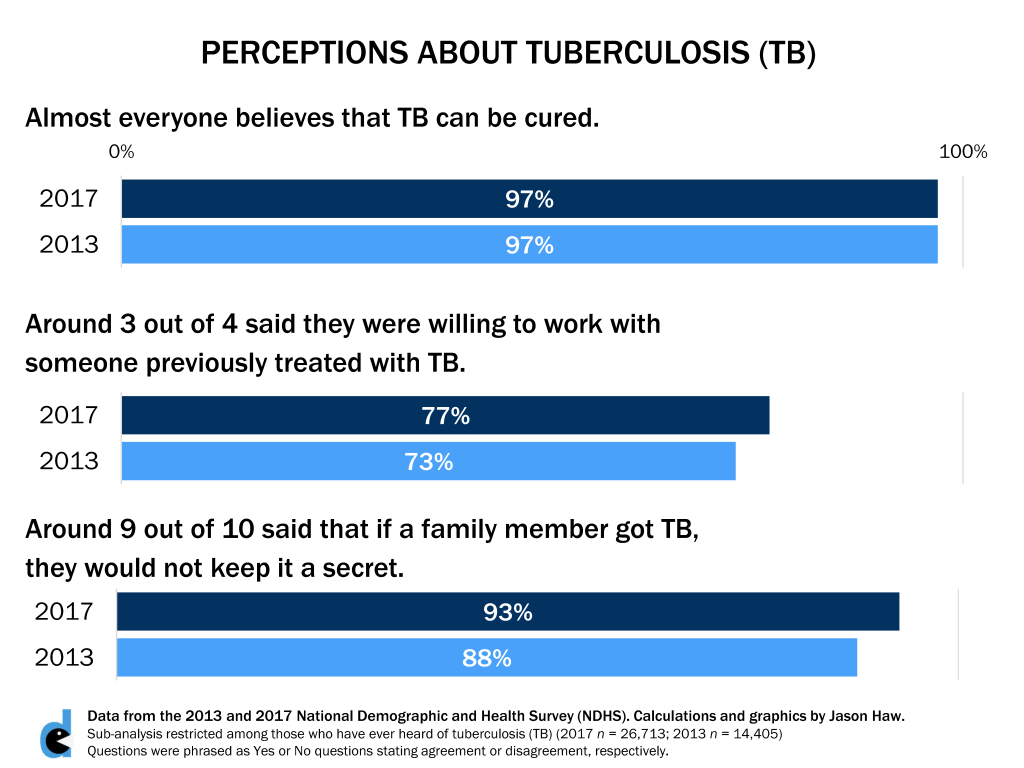
Around 3 out of 4 said that they were willing to work with someone previously treated with TB. It is important to note that someone who has been treated with TB is not infectious anymore, so there should be no cause for concern of anyone interacting with a TB patient that has already been treated and cured from TB.
The last question was phrased oddly, and the intention is not exactly clear. Around 9 out of 10 said they would not keep their family member’s TB a secret. This could be a question about addressing stigma, as family members may be transparent about the condition, but this could also be a question about patient confidentiality, where the family member has no right to disclose someone’s disease status. DHS may reconsider this question in future rounds.
All of my figures in this post and the rest of blog may be freely shared under Creative Commons 3.0 Attribution-Non Commercial-Share Alike.